New Ultrasound-Controlled Gene Therapy to Fight Cancer
Wang Lab and Pepper Workshop
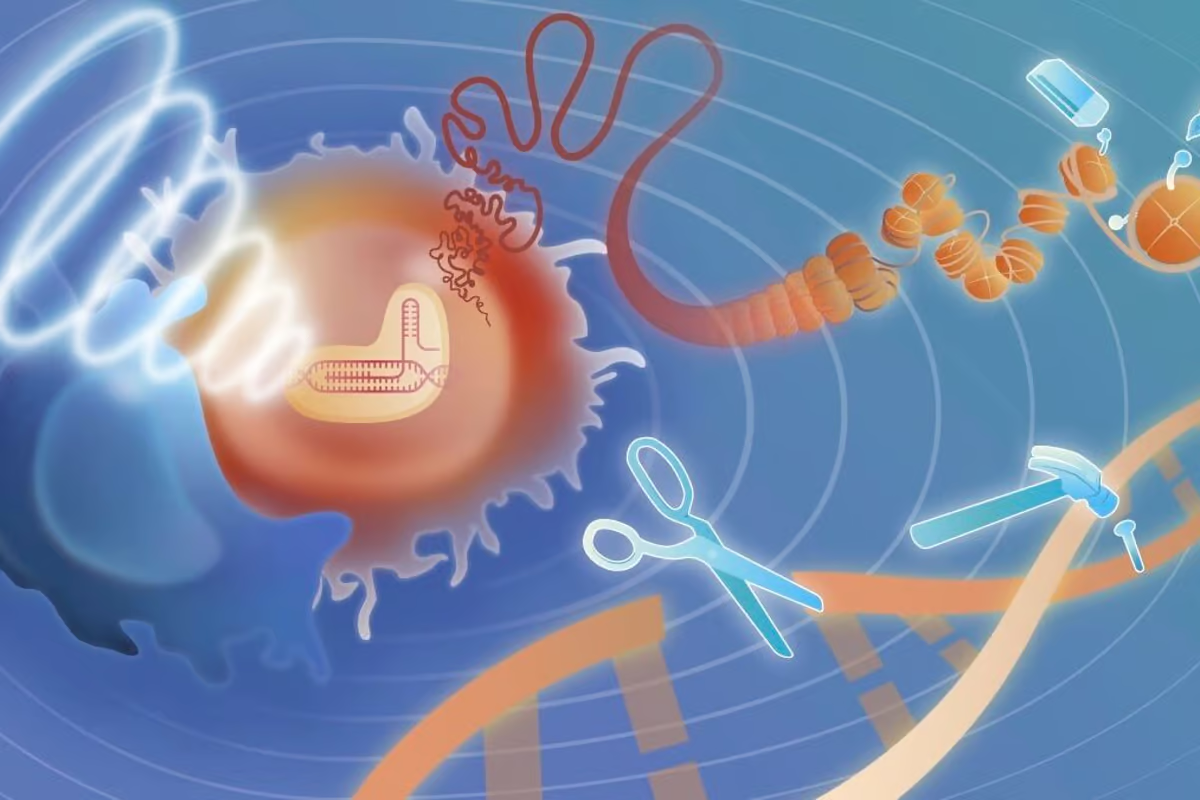
Researchers have developed an innovative gene therapy for cancer that can be remotely activated in specific areas of the body. The approach uses a version of CRISPR that responds to ultrasound pulses and has demonstrated effectiveness in eliminating tumors in mice.
CRISPR is a powerful gene-editing tool that employs the Cas9 enzyme to make precise edits to targeted genes. However, a key challenge is ensuring it operates only in the desired area, as prolonged activity outside the target zone can result in unintended edits and potentially trigger immune responses.
USC Scientists Achieve Precise CRISPR Control
Now, scientists at the University of Southern California (USC) have devised a method to control both the timing and location of CRISPR’s activation. In recent tests, the technique successfully eradicated tumors in mice.
In practice, CRISPR is delivered into the body via viral carriers and activated using ultrasound pulses targeted to specific regions. The mechanism relies on cells engineered to produce the Cas9 enzyme in response to heat, which is generated by the ultrasound.
With this controllable system, you can turn it on and off whenever needed,” explained Peter Yingxiao Wang, co-author of the study. “Once activated, CRISPR begins its work exactly where desired. After a set time, it deactivates on its own, but it can be reactivated later if necessary.”
Targeting Cancer Through Telomere Disruption
To target cancer, the CRISPR system was programmed to attack telomeres, the repetitive DNA sequences at the ends of chromosomes. This not only causes cancer cells to die but also triggers an immune response, summoning additional cells to assist in tumor elimination.
The treatment includes a second component using specialized CAR T cells. These immune cells are extracted from the patient, modified to attack specific targets, and reintroduced into the body. In this case, the target is a protein called CD19, which is highly expressed in certain types of cancer. CRISPR was also used to amplify the production of CD19, enhancing the therapy’s effectiveness.
Promising Results in Mouse Trials
In tests, mice with subcutaneous tumors treated with the combined CRISPR and CAR T therapy showed 100% survival and complete tumor eradication. By comparison, those treated with CAR T cells alone had a survival rate of just 40%.
While the results are promising, the therapy remains in early stages, and there is no guarantee the same outcomes will occur in humans. The researchers plan to refine the technique and explore applications beyond CAR T cell therapy in future studies.
Read the original article on: New Atlas
Read more: Cutting-Edge Sensor Technology Can Identify Lung Cancer Rhrough Your Breath










