What’s Next as Brain Implants Become Obsolete?

The significant progress in implantable neurological technology has provided relief for many individuals with neurological conditions, returning them to a semblance of normalcy. However, with its rapid evolution, there arises the question of what happens when these implants become outdated or if their manufacturer ceases operations.
Evolution of Implantable Neurological Devices
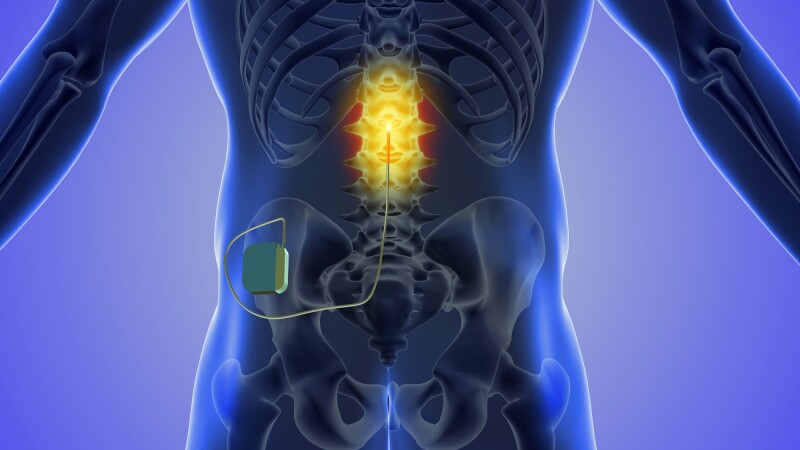
Remarkable advancements in medical technology have yielded increasingly sophisticated implanted neurological devices, including deep brain stimulation, vagal nerve stimulation, and spinal cord stimulators.
Among these innovations is Elon Musk’s Neuralink, a wireless brain-computer interface (BCI), which has garnered considerable attention. Moreover, China’s recent unveiling of its own BCI implant suggests a rapid advancement in the neurotechnological field, potentially challenging the dominance of the United States.
Depositphotos
Neurological technology implants have greatly improved the lives of individuals managing neurological disorders. Yet, as advancements progress rapidly, a pressing concern arises: what happens when these implants quickly become outdated or lose maintenance support from manufacturers, akin to obsolete operating systems like Windows? Is removal feasible, and if so, who bears the cost?
Advocates argue that safeguards must address these situations. A recent study by researchers at the Norman Fixel Institute for Neurological Diseases in Florida, US, proposed a formal definition of ‘implanted neurological device abandonment,’ emphasizing its pivotal role in shaping guidelines, policies, and laws concerning such devices.
Rita Leggett’s Journey with an Experimental Brain Implant for Epilepsy Management
In 2020, Nature Medicine featured Rita Leggett’s narrative. Leggett, an Australian, underwent an experimental brain implant to manage her epilepsy, effectively halting her seizures.
However, NeuroVista, the device’s manufacturer, folded during the trial due to investor apprehensions about supporting such invasive technology.
With the company’s closure, the implant remained inactive in Leggett’s head, although its battery was designed to last three years. Her husband’s attempt to acquire the device from NeuroVista was rejected due to its proprietary components. Consequently, her sole recourse was to have the device removed, or ‘explanted.’
Depositphotos
Frederic Gilbert, a neurotechnology ethics specialist at the University of Tasmania, notes that removing a device can equate to halting treatment, given the profound impact these devices have on a patient’s identity and the potential distress upon removal aligning with device effectiveness.
The study authors argue that clinical trial failure doesn’t necessarily equate to abandoning neurotechnological devices, as it could stem from safety concerns or ineffectiveness. They emphasize three criteria for trial management: informing participants of potential discontinuation, notifying them of trial cessation, and offering alternative treatments meeting standards.
Post-Trial Challenges in Neurotech Implant Management
Post-trials, managing neurotech implants poses challenges. While device removal is typically an option, coverage by health insurance is sought first. However, clear guidelines on whether to retain or remove the implant are lacking.
The global neurotechnology market is expected to reach US$17.1 billion by 2026, but this growth doesn’t guarantee the survival of companies. NeuroVista’s closure illustrates this uncertainty.
In 2019, Autonomic Technologies (ATI) ceased operations despite successful trials of its cluster headache stimulator. Regulatory fraud led to ATI’s downfall, leaving over 700 device users without access to crucial proprietary software for device maintenance. Fortunately, Unity HA acquired ATI’s intellectual property, earning FDA Breakthrough Device status in 2022.
Rachael Levy & Marisa Taylor/Reuters
In 2019, financial turmoil hit Nuvectra, a manufacturer of spinal cord stimulators, and Second Sight, a vision technology firm, ceased production of retinal implants to pivot toward brain implants.
This abrupt shift left around 350 recipients of Second Sight implants uncertain about their future. Later, Second Sight merged with Nano Precision Medicine. Additionally, Stimware, another spinal cord stimulator maker, recalled all devices in 2020 and filed for bankruptcy in 2022. Unfortunately, such closures are expected to continue.
When companies shutter, their implants typically remain in place due to the expense, risks, or lack of necessity associated with removal. Consequently, individuals with neurological conditions undergo a reset, albeit burdened with non-functional hardware.
If fortunate, individuals may seek a substitute device. A 2022 Nature article details that replacing outdated implants such as Nuvectra’s spinal cord stimulator requires weeks of recovery from surgery and is costly, totaling approximately US$40,000, assuming a replacement device is available.
The Rapid Evolution of Neurotechnology Devices
As previously mentioned, state-of-the-art neurotechnology devices can swiftly become obsolete, rendering them non-functional without ongoing maintenance and support.
In the summer of 2020, Elon Musk provided an update on the Neuralink implant, likening it to a “Fitbit in your skull.” He casually described the proposed insertion process for humans, which involves opening a section of the skull, inserting electrodes with a robot, and sealing the opening with super glue.
A highlight of the presentation was Dorothy the pig, previously implanted with a Neuralink. Musk showcased Dorothy’s implant removal as evidence of the device’s “reversibility.”
“Dorothy illustrates that with the Neuralink, one can undergo implantation, removal, and maintain a happy, healthy life, virtually indistinguishable from a normal pig,” Musk remarked.
Musk’s statement solely emphasized the positive outcomes of the device’s removal, omitting any discussion of potential risks. The full 2020 Neuralink progress update is accessible below.
Musk’s Venture Navigates FDA Approval Challenges
Musk’s brain implant venture has advanced from animal trials to preparing for its inaugural human trial, overcoming FDA obstacles for approval. Reuters reported in 2023 that the agency initially rejected the trial application due to safety concerns, notably regarding potential brain tissue damage during device removal. Musk has since obtained approval, indicating FDA satisfaction.
Expert opinions on the impact of removing Neuralink or comparable brain implants on brain tissue are scarce. It may be premature to speculate without human trial data. However, if implantation poses a risk of brain tissue damage, it’s reasonable to assume that removal carries similar risks.
The researchers conducted a thorough review of literature on neurological device abandonment to inform their study and reached a consensus on a suitable definition. They propose adopting a standardized definition, which includes one of the following options:
- Neglecting to disclose essential information regarding medical, technical, and/or financial responsibilities as integral components of patient consent during and after a clinical trial.
- Failure to meet reasonable obligations for medical, technical, and/or financial assistance before the end of the designated lifespan of an implantable device.
- Failure to attend to urgent requirements (e.g., infection or device reprogramming) of the individual utilizing the implanted device, potentially leading to safety issues and/or diminished device efficacy.
- The failure of a clinical research trial occurs when (1) informed consent neglects to cover ongoing access to and management of the implanted device (as outlined in 1 above) and/or other devices that may exhibit equal or superior therapeutic efficacy in the future, and (2) those overseeing the trial fail to make a reasonable attempt to ensure continued access to the device and support for patients benefiting from it.
Safeguarding Patients and Healthcare Providers in Rapidly Evolving Fields
The concerns outlined in this article highlight the necessity for enhanced and consistent guidance in this swiftly progressing domain to safeguard patients and their healthcare providers.
“We believe that the principles outlined above could serve as a starting point for further deliberation, discussion, and dialogue aimed at establishing a formal definition of abandonment of active implantable neurotechnological devices, along with guidelines, policies, and laws to prevent its incidence,” stated the researchers.
Read the original article on: New Atlas











Leave a Reply